
Scientists, medical professionals, and governments around the world are working to understand how the new respiratory disease ravaging Hubei province spreads—and how bad it could be for the rest of the world. Part of this effort is epidemiology: the study of how infections move through populations and how to control them.
Epidemiology incorporates everything from geography to complex mathematics in its effort to understand the spread of disease. Here are some basic epidemiological concepts that can help you get past the panic, misinformation, and xenophobia that tend to drive conversations around a newly emerging illness.
Spread it out
One quantity scientists use to measure how a disease spreads through a population is the “basic reproduction number,” otherwise known as R0 (pronounced “R naught,” or, if you hate pirates, “arr not”). This number tells us how many people, on average, each infected person will in turn infect. While it doesn’t tell us how deadly an epidemic is, R0 is a measure of how infectious a new disease is, and helps guide epidemic control strategies implemented by governments and health organizations.
If R0 is less than 1, the disease will typically die out: Each infected person has a low chance of passing the infection along to even one additional individual. An R0 larger than 1 means each sick person infects at least one other person on average, who then could infect others, until the disease spreads through the population. For instance, a typical seasonal flu strain has an R0 of around 1.2, which means for every five infected people, the disease will spread to six new people on average, who pass it along to others.
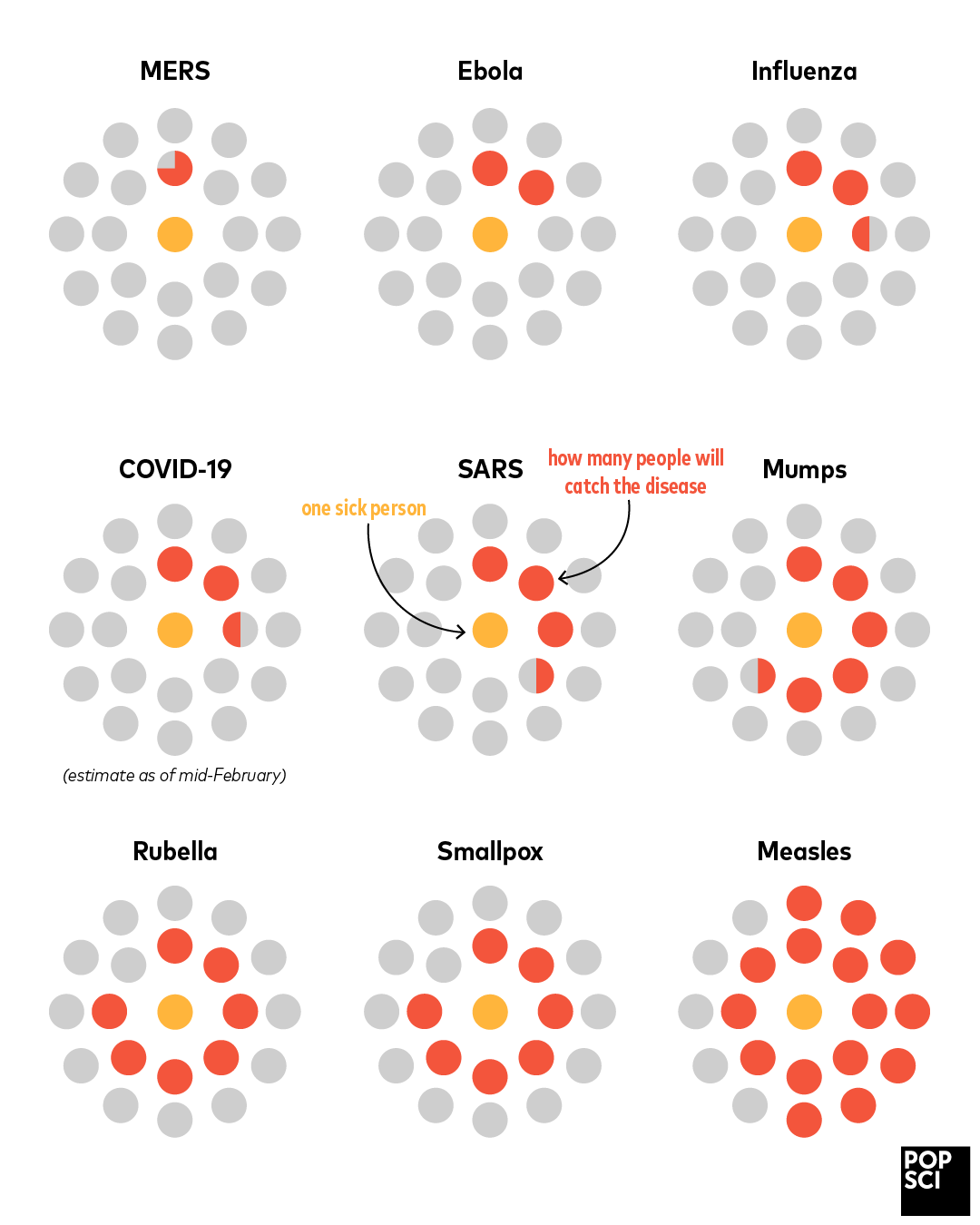
Measles is a champion disease in this respect. Its R0 is usually cited between 12 and 18, meaning each person with measles infects between 12 and 18 new people in an unvaccinated population. In the era before widespread vaccination, measles could easily sicken an entire school’s worth of children. Vaccinate your kids!
“Herd immunity” also depends on R0. The more people immune to a disease in a population, the fewer are available to be infected. If immunity reaches a critical level through vaccination or just naturally running out of new people to infect, the disease is starved out. Herd immunity is easier to achieve for lower R0 values because the disease doesn’t spread as readily.
But it’s important to remember that R0 is a statistical estimate of how a disease spreads in a particular population if it’s left unchecked. SARS and MERS both have higher R0 values (between 2 and 5) than the seasonal flu, but never spread widely enough to become worldwide epidemics. Flu, on the other hand, is always widespread despite having a relatively small basic reproduction number: the United States Centers for Disease Control (CDC) estimate between 3 and 11 percent of the US population gets sick with the flu every year.
That brings us back to the coronavirus now known as COVID-19. Because the disease is fairly new to medicine, researchers are still tabulating the data required to calculate R0 more or less in real time. As of February 19, 2020, estimates placed R0 above 1.4 but below 4, well within the range for other coronaviruses like SARS. (See this excellent Lifehacker article for more about the issues surrounding COVID-19 and R0.)
Deadly serious
Another important number for understanding diseases is the “case fatality rate” or CFR: What percentage of people who have a disease die from it? On one extreme, we have rabies, which has a 99 percent fatality rate if untreated. On the other is the common cold, which has a relatively high R0 but is almost never fatal (the exceptions being mostly immunocompromised people). The seasonal flu has a low CFR, but enough people get it every year that the CDC estimates as many as 30,000 Americans may have died from it between October 2019 and February 2020.
Similarly, measles is extremely infectious, but rarely fatal (though its spooky effect on the immune system can make victims susceptible to other life-threatening diseases). Smallpox was less infectious with an R0 of 5 to 7, but its CFR of roughly 30 percent made it devastating. Measles, though less serious, has such a high infection rate that it needs a much larger vaccinated population for proper herd immunity; smallpox vaccines achieved herd immunity at much lower rates, and wiped the illness out entirely by 1980.
The CFR for an emerging disease like COVID-19 is remarkably hard to estimate accurately, simply because all the numbers involved are relatively small. A preliminary calculation from February 8, 2020 estimates CFR of about 1.4 percent—meaning out of 1,000 infected people, around 14 will die—but that’s based only on cases from outside China, since the data from that nation’s government has been unreliable. The numbers will likely shift over the next weeks and months, but the CFR for COVID-19 seems to be lower than for SARS and MERS. However, the high concentration of cases in one region of China is putting a huge stress on the healthcare infrastructure, which is a concern for any major epidemic.
Knowing what we don’t know
Epidemiology is a game of “ifs” and approximations. Case fatality rates, basic reproduction numbers, and other quantities are derived from real-world data using mathematical models of disease. Because infections depend on a complex set of conditions, including things like weather and holiday travel, two outbreaks of the same virus might result in different-looking epidemics. That’s why R0 is usually given as a range of numbers and we hedge our language: not because our models are bad, but because reality itself is messy.
At the same time, epidemiology demystifies disease and guides how we deal with it. It both models how diseases jump from nation to nation in our interconnected age, and shows that citywide quarantines and travel bans don’t curtail the spread of an infection very much—while seriously disrupting the lives of the people who aren’t infected, along with their respective economies. And finally, epidemiology lets us compare COVID-19 to other epidemics, to inform us how bad it currently is and how widespread it might become if governments don’t handle it properly. We might not know everything about COVID-19 yet, but the knowledge from epidemiology helps us understand what it will take to beat it.
